Radiation Protection, Safety, Professionalism and Ethics
- Principles of radiation safety
- Radiation risk and epidemiological data
- Radiation protection regulations: NRC and Agreement States
- Radiation areas
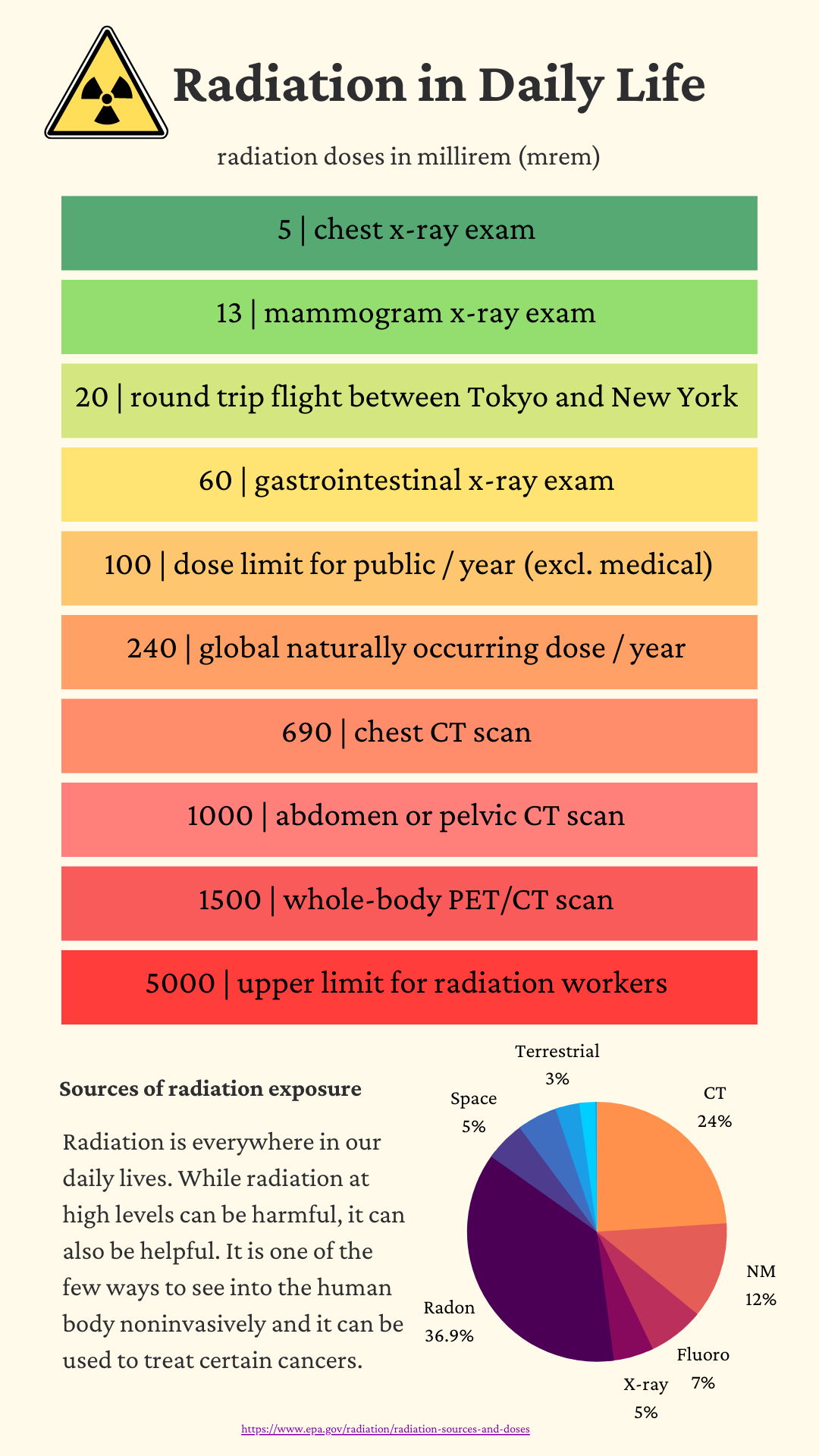
- Regulatory exposure limits
- Radiation protection program
- Radioactive source management and security
- Transportation of radioactive materials
- Shielding design for diagnostic, nuclear medicine and therapeutic installations
- Signage for diagnostic, nuclear medicine and therapeutic installations
- Non-ionizing radiation safety
- Mechanical and electrical safety
- Principles of quality assurance and quality control
- Management of radiation accidents and large-scale radiological events
- Professionalism and ethics
Principles of radiation safety
 ALARA - As low as reasonably achievable
ALARA - As low as reasonably achievable
Dose reduction through distance (inverse square law), shielding, and time
- Distance - inverse square law means doubling distance from radioactive source results in 1/4 dose.
- Shielding - materials that can block radiation (e.g. concrete, lead, leaded glass, l-blocks) reduce dose depending on their HVL.
- Time - Dose is cumulative, so the less time spent near a radioactive source, the less exposure/dose to the individual. Work efficiently.
Try to stay below 10% of the regulatory dose limits.
Radiation risk and epidemiological data
Dose Equivalent: Include differences in biological effects for radiation of different "quality"
$H = D \cdot Q$ where D is absorbed dose and Q is quality factor based on radiation type. Unit of Sievert: Sv = J/kg = 100 rem.
Similar to RBE in radiation biology, but more generic.
Q-values:
- Photons: 1
- Protons: 2
- Alpha: 20
- Neutron < 10 keV: 5
- Neutron 10 - 100 keV: 10
- Neutron 0.1 - 2 MeV: 20
- Neutron 2 - 20 MeV: 10
- Neutron > 20 MeV: 5
Effective Dose
Effective dose - tissue weighting table
Effective dose equivalent: $H_E = \sum{W_T H_T}$, sum of tissue-weighted equivalent doses.
Committed effective dose equivalent (CEDE): effective dose over 50 years due to ingestion/inhalation.
Deterministic: known effects, with severity depending on effective dose. Latency of days to weeks
< 0.1 Gy. no deterministic effects known
Stochastic: unknown when/what effects will occur, severity does not depend on dose, but likelihood does (as does tissue type irradiated). Latency of years (5-15 Leukemia, 20-60 solid tumors)
No threshold on stochastic effects (based on Linear No Threshold (LNT) model)
1 Gy needed to double spontaneous mutation rate
Parallel Functional Subunits (FSU): Each FSU can operate independently. One fails then system declines a bit, but functions
e.g., Kidneys, Liver
Serial FSU: One FSU out affects others
e.g., GI tract, Spine
|
Tissue Weighting factor |
|||
|
Tissue |
NRC (2011) |
NCRP115 |
ICRP103 |
|
Bladder |
– |
0.05 |
0.04 |
|
Bone marrow (red) |
0.12 |
0.12 |
0.12 |
|
Bone surface |
0.03 |
0.01 |
0.01 |
|
Brain |
– |
– |
0.01 |
|
Breast |
0.15 |
0.05 |
0.12 |
|
Colon |
– |
0.12 |
0.12 |
|
Esophagus |
– |
0.05 |
0.04 |
|
Gonads |
0.25 |
0.20 |
0.08 |
|
Liver |
– |
0.05 |
0.04 |
|
Lung |
0.12 |
0.12 |
0.12 |
|
Salivary glands |
– |
– |
0.01 |
|
Skin |
– |
0.01 |
0.01 |
|
Stomach |
– |
0.12 |
0.12 |
|
Thyroid |
0.03 |
0.05 |
0.04 |
|
Subtotal |
0.70 |
0.95 |
0.88 |
|
Remainder |
0.30 |
0.05 |
0.12a |
|
Total |
1.00 |
1.00 |
1.00 |
Dose Threshold for Deterministic Effects* |
||
| Tissue | Total acute dose threshold (Gy) | Time to develop effect |
| Lens of Eye | ||
| Detectable opacities | 0.5–2 | > 1 year |
| Cataract formation | 5.0 | > 1 year |
| Skin | ||
| Skin reddening | 3–6 | 1–4 weeks |
| Temporary hair loss | 4 | 2-3 weeks |
| Skin death and scarring | 5-10 | 1-4 weeks |
| Testes | ||
| Temporary sterility | 0.15 | 3-9 weeks |
| Permanent sterility | 3.5–6 | 3 weeks |
| Ovaries | ||
| Permanent sterility | 2.5–6 | < 1 week |
| Gastrointestinal | ||
| Mucosa lining loss | 6-10 | 6-9 days |
| Bone Marrow | ||
| Reduction of blood cell production | 0.5 | 1-2 months |
| CNS | ||
| Seizure, unconsciousness | 30 | hours |
| * 1% incidence level based on ICRP publication 103 (2007) | ||
Timeline:
- prodromal
- Within minutes/hours
- vomiting/diarrhea, slight headache
- latent
- no symptoms
- abnormal lab work
- longer for lower doses
- 21-35 days for 1 Gy
- < 7 days for 6 - 8 Gy
- manifest illness
- hematopoietic syndrome, fatigue, weakness
- GI syndrome for dose > 5 Gy,
- cerebrovascular syndrome for dose > 20 Gy
- recovery or death
- Depends on total dose, dose rate, dose distribution
Higher doses → Faster onset of symptoms, shorter overall timeline
Excess relative risk (ERR): proportional increase in risk from exposure relative to background risk. Higher for children (high growth rate)
8.6%/Sv (male) and 12.8%/Sv (female)
|
|
Dose limits to workers and public |
||
|
Occupational |
Location |
Dose (mSv/yr) |
Dose (rem/yr) |
|
Continuous/frequent |
50 mSv/yr |
5 rem/yr |
|
|
Cumulative dose |
20 mSv/yr over 5 yrs, 10*age |
2/yr over 5 yrs 1*age |
|
|
Infrequent |
50 mSv in one year |
5 rem in one year |
|
|
Lens of eye |
150 mSv/yr |
15 rem/yr |
|
|
Skin, hands, feet |
500 mSv/yr |
50 rem/yr |
|
|
Fetus |
5 mSv/gestation (0.5/mo) - NCRP |
0.5 rem/gestation |
|
|
Minor |
10% of adult limit |
||
|
Public |
General Public |
1 mSv/yr |
0.1 rem/yr |
|
Unrestricted areas |
0.02 mSv/hr |
0.002 rem/hr |
|
Shallow dose equivalent (i.e., skin dose) is measured to 0.007 cm over an area of 1 square cm (NRC).
Lens dose measured to depth of 0.3 cm.
Deep dose equivalent is measured to 1 cm.
Monitoring is required (NRC) if worker likely to receive 10% of annual limit
Monitors worn on torso, and possibly ring if handling sources.
Increased risk as a function of dose:
- Hereditary: 1%/Sv
- Acute exposure: 10%/Sv
- Chronic exposure: 5%/Sv
Fetal doses
TG-36 (1995): Fetal Dose from Radiotherapy with Photon Beams
Considerations for peripheral dose outside beams:
- Head leakage
- Scatter from head (collimators, modifiers)
- Scatter from patient
- Neutrons (beams > 10 MV)
At about 30 cm, scatter in the patient and head leakage are approximately equal.
Beyond 30 cm from the primary beam, head leakage predominates.
Scatter from wedges (and other blocking devices) increases the dose near the beam edge by a factor of 2 to 5.
At 10 cm from the field edge the dose is about 1% the central axis value
At 30 cm from the field edge the dose is about 0.2% the central axis value
Use lower energy beams (< 10 MV) if possible, incase of photoneutrons (NCRP considered negligible)
Adverse effects: malformations, mental retardation, later cancer (leukemia).
Risk by dose:
- < 5 cGy, little risk at any stage
- 5-10 cGy, risk is uncertain
- 10-50 cGy, significant risk, especially first trimester
- > 50 cGy, high risk, any trimester
- 100 cGy, kills 50% of fetuses.
Risk by stage:
- Preimplantation (1st week), risk: death of embryo.
- Embryonic (1-8 weeks), risk: malformation of specific organs, growth retardation, sterility.
- Early fetal (8-15 weeks), risk: severe mental retardation and small head syndrome (SHS).
- Mid-fetal (15-25 weeks), risk: severe mental retardation.
- Late fetal (>25 weeks), risk: probably subsequent cancer development.
Mitigation in radiation therapy
- Lower energies (< 10 MV)
- Modify field and angle, split beams
- 3D-CRT instead of IMRT to reduce head leakage from higher MUs
- Special shielding (bridge) around abdomen/fetus
- Minimize alignment imaging
- TLDs for in-vivo dosimetry
Personnel Dosimetry
Monitoring devices required if worker likely to receive > 100 mrem (>1 mSv) in a year.
Badge types: Film (no longer common), OSL (optically stimulated luminescence), TLD (thermoluminescent dosimeter)
Torso (chest/collar) badge and ring badge in index of dominant hand. Abdomen badge for declared pregnant workers.
Radiation exposure causes electrons to be trapped in scintillation like material. Stimulate optically or thermally to release electrons, measure light, correlate to dose (must be calibrated).
Exposure records should be reviewed monthly.
ALARA: < 10% of NRC limit (whole body: 5 rem/yr = 50 mSv/yr, skin/extremity/organ < 50 rem/yr = 500 mSv/yr)
Level 1: > 10% and <30% of NRC limit, RSO investigates safety practices
Level 2: > 30% NRC limit, RSO required to take action to ensure limits are not reached
Level limits specified by department/RSO.
Retain records indefinitely (duration of license).
Internal doses
Medical Internal Radiation Dose (MIRD) - dose from internal source (accidental or deliberate from diagnostics or treatments)
Ingestion, inhalation, injection, absorption.
$D(r_T) = \sum_s{\tilde{A}_s(r_s) S(r_T ← r_s)} = \sum_s{\tilde{A}_s(r_s) \sum_i{\Delta_i \phi_i / m_T}}$ where $\tilde{A}_s = A_0 F T_{eff}$ is the time integrated activity, the s-factor is specific to radionuclide (mean dose to target organ given integrated activity in source organ). Sum over mean energies, $\Delta_i$ for each ith radiation times fraction absorbed by target (depends on radiation type and size and anatomy) divided by the mass of the target organ.
$\tilde{A}_s \Delta$ is the total energy from source organ. $\phi$ is fraction of source energy absorbed by target. $1/m_T$ to give energy / mass = dose.
$\phi = 1$ when source is also target (alpha and beta particles, short range).
Reference man/woman and computer models (digital phantoms) of organ locations are used to estimate doses. E.g. $S(r_T ← r_s)$ is tabulated.
Monitoring is required (NRC) if worker likely to receive 10% of annual limit on intake.
Bioassays may be needed: urine, stool, external detectors (if gamma rays present).
Intake activity = bioassay activity / Intake retention factors. IRF are tabulated by nuclide and time.
Mitigation
Reduce absorption and deposition
- Iodine: potassium iodine to block thyroid deposition of radioactive iodine
- Rare earths: Zn-DTPA to chelate
- Plutonium: Ca-DTPA to chelate
- Uranium: bicarbonate to alkalinize urine
- Cs, Ru, Tl: Prussian blue (ferrous salts) to block GI absorption
- Tritium: water, dilution
Increase elimination and excretion
- Catharsis - administering an agent that accelerates defecation
- Gastric lavage - stomach pumping and irrigation
- Rinsing nasal passages
Derived air concentration (DAC): maximum permissible air concentration of a radionuclide that if inhaled by a worker over the course of a year (2000 hours) would result in them reaching the ALI.
Radiation protection regulations: NRC and Agreement States
Nuclear Regulatory Commission (NRC) was created to ensure the safe use of radioactive materials while protecting people and the environment.
NRC: power plants, large quantities of nuclear material, storage of high-level waste.
NRC or Agreement States: byproducts, source materials, other special materials
States:
– radiation-producing machines, such as X-ray machines (both medical and industrial)
– particle accelerators
– radioisotopes (such as cobalt-57) produced on particle accelerators
– all naturally occurring radioactive materials (such as radium and radon)
Agreement states have their own regulations that are at least as strict as NRC.
NRC documents
- 10 CFR 20 (Standards for Protection Against Radiation).
- 10 CFR 35 (Medical Use of Byproduct Material).
- 10 CFR 71 (Packaging and Transportation of Radioactive Materials).
- NUREG 1556 gives limits for releasing radioactive patients after therapy.
Restricted area: access controlled by licensee to protect against exposure
Controlled area: outside restricted area but limited access, RSO oversight
Radiation area: possible to receive > 0.05 mSv in 1 hour at 30 cm from source or shielding
High radiation area: possible to receive > 1 mSv in 1 hour at 30 cm from source or shielding
Very high radiation area: possible to receive > 5000 mSv in 1 hour at 1 m from source or shielding
All containers should specify type and quantity of radioactive material.
Notify NRC if dose exceeds 5× the allowable limits:
total effective dose equivalent (TEDE) exceeds 250 mSv, lens exceed 750 mSv, over 5× ALI over 24 hours, shallow dose > 2500 mSv, loss of radioactive material in excess of 1000× specified limits.
Notify NRC within 24 hours if individual receives TEDE or shallow dose in excess of annual limits within 24 hours, or release of material such that ALI could be exceeded in 24 hours.
Notify NRC within 30 days if loss of radioactive material 10× specified limit.
All sites must have Radiation Safety Officer (RSO) and Radiation Safety Committee (RSC)
Establish radiation safety program
Keep records and ensure compliance of licenses, authorized users (physicians) and physicists, storage and inventory, occupational doses, patient release surveys, and waste disposal records.
RSC must meet quarterly with RSO, AMP, AU, rad onc nurse and review safety program.
Quarterly checks:
ALARA level 1: 10% of allowed limits, check if appropriate
ALARA level 2: 30% of allowed limits, investigate, try to reduce
ALARA exceeded: 40% and written documentation, 70% and action to change work environment
10 CFR 35 (Medical Use of Byproduct Material):
Written Directive:
- Must be dated and signed by an authorized user.
Should include: - Name
- Dosage (including total and dose per fraction)
- Route of administration
- Type of material/radionuclide
- Treatment site
- Number of sources used and their strength (for LDR)
Medical Event (this is the new term for a mis-administration) is when:
- Wrong patient is treated.
- Wrong radionuclide is used.
- Using a leaking source.
- Wrong delivery method is used.
- If the patient’s total dose differs from the prescription by more than 20%.
- If a single fraction dose differs from the prescription by more than 50%.
Release of Radioactive Patients (NUREG 1556 appendix U):
Limits depend on the radionuclide that has been used.
Keep exposure to members of the public below 5 mSv from the implant.
Note: this is above the normal public limit of 1 mSv as the level is raised automatically to 5x the limit by the NRC for outpatient medical procedures involving radiation.
- For I-125 prostate seed implants the recommended release criteria is <1 mR/h at 1 meter.
- For Pd-103 prostate seed implants the recommended release criteria is <3 mR/h at 1 meter.
- For I-131 thyroid ablation patients the recommended release criteria is <7 mR/h at 1 meter.
(shorter half life allows for higher initial limit)
Regulatory exposure limits
Typical background yearly dose: 6.2 mSv. Roughly 50% natural background and 50% medical (over population)
Occupational
Annual limit: 50 mSv = 5 rem
Cumulative dose: 10 mSv x age in years
Annual limit to eye: 150 mSv = 15 rem
Annual limit to shallow (skin, hands, feet): 500 mSv = 50 rem
General public
Annual limit: 1 mSv is continuous, 5 mSv is infrequent
Annual limit shallow: 50 mSv
Fetus
Pregnancy duration: 0.5 mSv/month (only if officially declared)
Uncontrolled areas
Continuous exposure limit: 0.5 μSv/hr (1 mSv/yr)
Transient exposure limit: 20 μSv/hr (50 μSv/hr trigger level)
Controlled areas
Exposure limit: 50 mSv/yr (ALARA goal of 5 mSv/yr)
Personnel Monitoring
If dose likely to be < 10% of limits, monitoring not needed. (< 1 mSv expected if pregnant)
Worker dose from intake is low, no monitoring.
Diagnostics and unsealed treatments
Na131I - > 30 μCi considered therapy, need written directive. Also any unsealed therapeutic byproduct material (32-P, 90-Y).
Fetus: >15 rad associated with defects, < 5 rad negligible.
Infant: Per NRC, written instructions to breast feeding women if likely to exceed 5 mSv = 500 mrem. Oral instructions if dose likely to exceed 1 mSv = 100 mrem. (From ingestion or proximity.)
NRC guides maximum/mimimum activity administered and dose rate at 1 m (mSv/hr) at which patients may be release and given instructions.
NRCP report 37 provides equation for calculation of exposure for time t and distance r from a radioactive patient.
$$ D(t) = \frac{34.6\, \Gamma\, Q_0\, T_p\, (1-e^{-ln(2) t /T_p})}{r^2}$$
where 34.6 = 24 hrs/day * decay integration of 1.44, $\Gamma$ is specific gamma ray constant for point source in R/mCi-hr at 1 cm, $Q_0$ is initial activity in mCi at release time, $T_p$ is physical half-life in days, $r$ is distance form point source to interest point in cm, $t$ is exposure time in days.
Conservatively, assume exposure is dose to total decay → $(1-e^{-ln(2) t /T_p}) = 1$
For isotopes with > 1 day half-life, can assume average of 25% occupancy at 1 meter→ $(1-e^{-ln(2) t /T_p}) = 0.25$
Biological decay is not accounted for.
Patients may be released without record if the administered activity s below the allowed activity according to column 1 of table 1 in the NRC docs. Patients may be release with record if activity remaining is below that in column 1 of table 1. e.g. 33 mCi of I-131. Record always required if breastfeeding.
Patients may be released with record if dose rate at 1 meter no greater than column 2 of table 1 for the given radionuclide. e.g. 0.07 mSv/hr = 7 mrem/hr for I-131.
Records required if dose calculation uses retained activity, occupancy factor less than 0.25 at 1 meter, effective half-life or shielding my tissue (10 CFR 35.75(c)).
Exposure rate: $\frac{\Gamma\, A}{d^2}$ where $A$ is the activity, $d$ is distance from source, and $\Gamma$ is the gamma constant, specific to each radionuclide. Applies to a point source of a gamma-emitting radionuclide.
Rate is typically given in R/hr, and $\Gamma$ is in units of R-cm2 / mCi-hr.
Radioactive source management and security
Stored so that public will not receive more than 1 mSv in a year. Dose in unrestricted area < 0.02 mSv averaged over an hour.
E.g., 6.5 mCi of I-131, 19 mCi of Ga-67, 19 mCi of Tc-99m would have to continuously irradiate an individual without shielding. Dose rate would be < 0.057 mrem = 0.57 μSv.
Must report to NRC lost or stolen radioactivity if over 10x amount listed in NRC Part 20, Appendix C
Radiation Transport
Shipping regulations governed by DOT. Radioactivity is category/hazard class 7.
TI, transportation index (given without units): Level of radiation at 1 m from package surface, in mrem/hr.
Specifies degree of caution needed during transport.
White I: ≤ 0.5 mrem/hr at surface, not detectable at 1 meter
Yellow II: ≤ 1 mrem/hr at 1 meter AND ≤ 50 mrem/hr at surface
Yellow III: > 1 mrem/hr (< 10 unless special) at 1 meter OR > 50 mrem/hr at surface (< 200 unless special)
Special form radioactive material: single solid piece, approved sealed source
Normal form RAM: not special form, e.g., liquid or gases
Special nuclear material: enriched U or Pu
Source material: U or Thorium
Package types:
Type A if activity between 0.001A and A (applies to nuclear medicine)
A1: special form
A2: normal form, Marked "Radioactive Material Type A Package, UN 2915"
Type B if activity between A and 3000A (potentially life endangering amounts)
Value of A depends on material type
Receiving: test within 3 hours (wipe tests over 300 cm2). Package inspected visually for damage.
Wipe tests action limits: Alpha 22 dpm/cm2, beta/gamma 220 dpm/cm2
→ 6600 dpm over the 300 cm2 for alpha, and 66000 dpm over 300 cm2 for beta/gamma
Survey at surface and one meter, should not exceed TI on placard.
Radioactive waste should be decayed in (shielded) storage for 10 half-lives, document background reading before disposal.
Shielding design for diagnostic, nuclear medicine and therapeutic installations
NCRP 147 - Structural Shielding Design for Medical X-ray Imaging Facilities
TG-108 - PET and PET/CT Shielding Requirements
Restrictions:
Controlled area: 5 mGy/year or 0.1 mGy/week
Uncontrolled area: 1 mGy/year or 0.02 mGy/week
No more than 20 μSv in any 1 hour
Barrier thickness: $B = \frac{P d^2}{WUT}$ - see therapeutic section
Number of TVLs: $n = -\text{log}(B)$
X-ray machines have same recommendations as for therapy suites: P = 0.1 mSv/wk controlled, P = 0.02 mSv/wk uncontrolled:
$B = \frac{P \cdot d^2}{WUT}$ for primary radiation
B = the barrier transmission factor (reading attenuated divided by open).
P = the dose per week required outside the barrier for protection (units Sv/wk).
d = the distance from the x-ray target to a point 0.3 m beyond the wall.
W = the workload, defined as the unshielded air-KERMA rate per patient times the number of patients treated in 1 week (typical 5 mGy/pt, 50 pt/wk, about 250 mGy/wk).
U = the use factor, fraction of the time per week that the primary beam falls on the barrier (assumed to be 0.25 for conventional simulators).
T = the occupancy factor, the fraction of time that the maximally exposed individual will be in the area outside the barrier per week. NCRP-147 values 1 for offices, 1/2 exam rooms, 1/5 corridors, 1/8 doors, 1/20 public areas, 1/40 outdoors, stairs, closets, etc
Penetration power depends greatly on kVp: ×3 from 60 to 100 kVp, ×8 for leakage
→ need to adjust workload
Leakage: 1 mSv/hr at 1 meter using highest kVp and mA.
Typically, the only shielding requirements for a x-ray machine (e.g., simulator) is 1/32 in (0.8 mm) of lead.
Need more for fluoroscopy.
CT: $B = \frac{P}{WDT}$, where workload is defined as mA-min/wk, D is dose/scan or mA-min per scan.
Manufacturers often give isodose maps around machine.
Typically, the shielding requirements for CT is 1/16 in (1.6 mm) of lead.
PET/CT: $B = \frac{P \cdot d^2}{WUT}$
Use factor assumed 1 (isotropic)
Workload depends on number of patients $n$, injected dose $A$, uptake time $t$, gamma factor for F-18.
$W = A \Gamma n t$ where $\Gamma_{F18} = 5.29 \text{mSv-cm}^2\text{/ mCi / hr}$
Typically, the shielding requirements for PET is about 1 cm lead.
More details on NM/PET page
Signage for diagnostic, nuclear medicine and therapeutic installations
Unrestricted: general public, exposure limit < 2 mrem/hr (< 0.02 mSv/hr)
"Restricted area: authorized individuals only" (sign required), exposure > 2 mrem in an hour.
"Caution: Radioactive Materials Area", area where radioactive materials are stored or used. Area surveys and wipe tests required.
"Caution: Radiation Area", imaging/treatment rooms, possibility of person exposed to > 25 μSv/hr
Management of radiation accidents and large-scale radiological events
Spills
Major if: I-131 > 1 mCi, Ga-67, In-111, I-123 > 10 mCi, andTc-99m, Tl-201, Tl-201 > 100 mCi.
Procedure:
- Notify everyone in the area.
- Prevent the spread of contamination. Remove contaminated clothing. If individual is infected wash with lukewarm water and soap.
- Notify RSO
- Wearing appropriate protective gear, clean up the spill.
- Survey area/wipe test, if necessary clean again. If contamination can’t be fully cleaned, use appropriate signs and block the area.
- Check self for contamination.
- Report incident to RSO if contamination is found on individual.
Numbers to remember
Q values: 1 photons, 2 protons, 20 alphas, ~10 for unknown neutrons
Rough levels of whole body radioactivity for various effects:
- Hematopoietic: ≥ 0.5 Gy
- Erythema: ≥ 3 Gy
- Sterility: ≥ 3 Gy
- GI: ≥ 6 Gy
- CNS: ≥ 20 Gy
Dose limits:
Worker, whole body: 50 mSv/yr (1 cm deep)
Worker, eye: 150 mSv/yr (0.3 cm deep)
Worker, shallow: 500 mSv/yr (0.007 cm deep)
Worker, fetus: 5 mSv/gestation
Worker, minor: 10% of adult
Public: 1 mSv/yr
Unrestricted areas: 0.02 mSv in any hr, 0.02 mSv/wk
Excess relative risk: ~ 10%/Sv
Transport:
White: < 0.5 mrem/hr at surface
Yellow II: ≤ 1 mrem/hr at 1 meter, < 50 mrem/hr at surface
Yellow III: > 1 mrem/hr at 1 meter (< 10 unless special)